Implant Tech Aims for 50% Fewer Cancer Deaths
Written by Shaveta Arora, Arushi Sharma
Cutting-edge implant technology is setting ambitious goals, aiming to achieve a remarkable 50% reduction in mortality rates across various medical fields. These advancements hold the promise of significantly improving patient outcomes and saving lives.
A team of scientists led by Rice University in the United States has received $45 million in funding to develop implant technology that has the potential to cut cancer deaths by more than half. The grant, which was given to researchers from seven different states, will help to accelerate the development and testing of a novel cancer therapy approach. This strategy aims to significantly improve the efficacy of immunotherapy for patients suffering from difficult-to-treat tumors such as ovarian, pancreatic, and other cancers.
"Instead of tethering patients to hospital beds, IV bags, and external monitors, we'll use a minimally invasive procedure to implant a small device that continuously monitors their cancer and adjusts their immunotherapy dose in real-time," Rice bioengineer Omid Veiseh, the principal investigator (PI) on the ARPA-H cooperative agreement, said in a statement.
Closed-loop therapy, previously utilized in diabetes management, brings about a revolutionary shift when applied to cancer immunotherapy. This innovative approach maintains continuous communication between an insulin pump and glucose monitor.
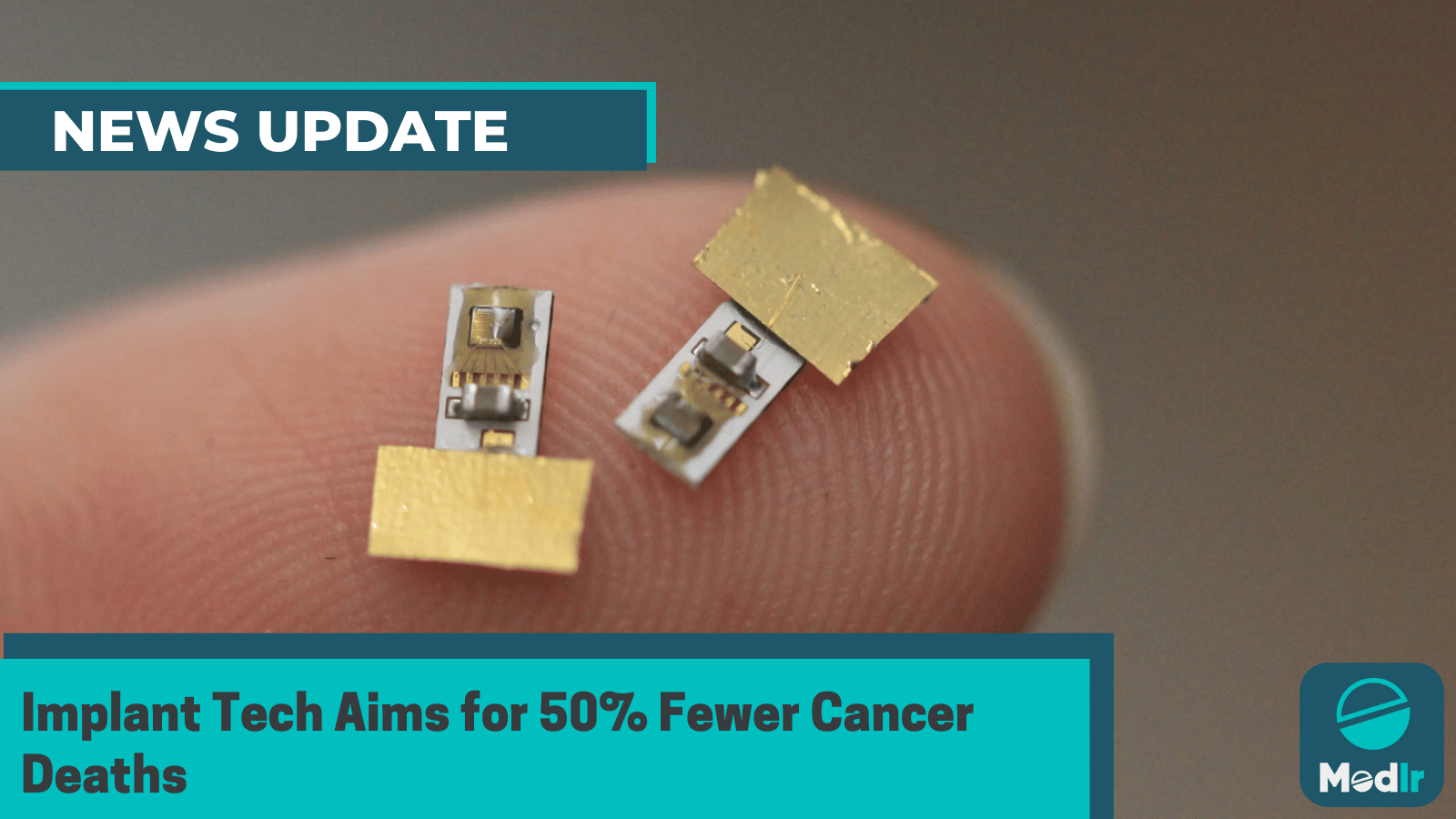
Engineers, healthcare professionals, and a wide range of specialists from fields such as synthetic biology, materials science, immunology, oncology, electrical engineering, and artificial intelligence make up the team. The collaborative effort is known as THOR, which stands for "targeted hybrid oncotherapeutic regulation," and its team has created an implant known as HAMMR, which stands for "hybrid advanced molecular manufacturing regulator."
"Cancer cells are continually evolving and adapting to therapy. However, currently available diagnostic tools, including radiologic tests, blood assays, and biopsies, provide very infrequent and limited snapshots of this dynamic process," Dr. Amir Jazaeri, a co-principal investigator and professor of gynecologic oncology at the University of Texas MD Anderson Cancer Center, said in a statement.
"As a result, today's therapies treat cancer as if it were a static disease. We believe THOR could transform the status quo by providing real-time data from the tumor environment that can in turn guide more effective and tumor-informed novel therapies," he added.
"The technology is broadly applicable for peritoneal cancers that affect the pancreas, liver, lungs, and other organs," said an associate professor of bioengineering at Rice.